Antibody production
Antibody production
Will a single COVID-19 drug be enough to treat all patients?
As more and more biotherapeutics enter the early stages of clinical development, scientists are questioning if current approaches will be sufficient to curb the pandemic. On the one hand, anti-inflammatory and immunosuppressant drugs, that benefit only a subgroup of patients, are leading the race for clinical approval. On the other hand, anti-SARS-CoV-2 antibodies are mostly focusing on a single region of the virus, severely compromising our chances of finding the best candidates.
The “first” wave of lifesaving COVID-19 drugs
In mid-June, dexamethasone became one of the first drugs shown to improve the survival of COVID-19 patients on ventilators. But the drug, an inexpensive corticosteroid with anti-inflammatory and immunosuppressant effects, is also widely used to treat rheumatoid arthritis, asthma, and some forms of cancer.
As we saw for hydroxychloroquine and chloroquine, the announcement of this repurposed drug’s success caused a spike in demand leading hospitals to experience severe shortages. This disruption is further compromising physicians’ ability to treat COVID-19 patients and others who depend on the regular prescription of this drug to treat other conditions.
The same is not likely to happen with Levilimab, an anti-inflammatory chimeric humanized antibody (camelid/human) that received state approval in Russia for the treatment of COVID-19. Despite its anti-inflammatory properties, unlike dexamethasone, Levilimab has yet to be licensed to treat other diseases. Suggesting that, for the moment, its production will solely aim at supplying the growing demand for COVID-19 drugs.
More than 40 other antibodies are currently undergoing clinical trials (phases 1, 2, and 3) to determine safety and efficiency in the treatment of the COVID-19 disease. Most of the frontrunners are repurposed anti-inflammatory drugs with interleukin or complement blocking activity. But despite the recent successes achieved by Levilimab and dexamethasone, these anti-inflammatory treatments are designed only to alleviate inflammation in a subgroup of COVID-19 patients.
Studies show that this subgroup of COVID-19 patients presents high levels of pro-inflammatory cytokines (interferon-gamma and some interleukin molecules) and chemokines (CXCL10 and CCL2). These levels have also been associated with increased pulmonary inflammation and subsequent damage resulting from an aberrant immune response.
But a second “wave” of drugs will likely dominate clinical trials in the upcoming months – COVID-19 drugs with antiviral neutralizing activity.
The second “wave” of lifesaving COVID-19 drugs
The fact that the first “wave” of COVID-19 drugs focuses mostly on fighting the exacerbated inflammatory response can be easily explained. Inflammation in the form of a cytokine storm has been previously observed in other infectious diseases, such as the ones caused by MERS-CoV and different strains of influenza. These drugs also work as immunosuppressants and, thus, are useful to treat autoimmune diseases such as rheumatoid arthritis.
Since inflammation is a symptom that COVID-19 shares with other diseases, we already have at our disposal a plethora of different drugs that can be repurposed for the treatment of the new disease. However, the second “wave” will represent an important shift from the easily available symptomatic treatments towards highly specific treatments.
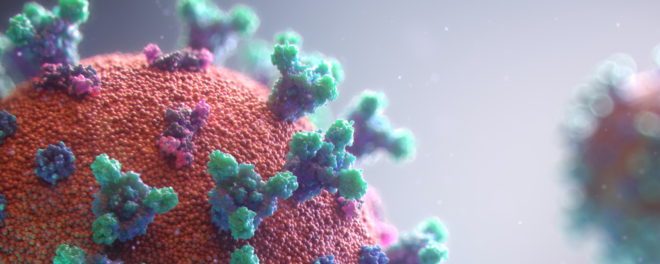
Presently, almost 100 COVID-19 drugs are currently in the discovery phase and preclinical evaluation. Of these, more than 80 drugs target the spike protein of SARS-CoV-2. Thanks to the early efforts of countless researchers, it is well-established that the spike protein of SARS-CoV-2 consists of two subunits – S1 and S2 – linked by a furin cleavage site.
The two subunits of the spike interact with our epithelial cells in a concerted manner. The first subunit (S1) binds the ACE2 receptor via its receptor-binding domain (RBD) and causes the cleavage of the spike. This further causes a structural shift in the spike exposing the protein machinery responsible for membrane fusion (S2) and viral internalization. Being the point of entry of the virus, the spike protein and, particularly, the receptor-binding domain (RBD), became the preferred targets for the development of highly specific therapeutics.
Current anti-spike drugs are mostly monoclonal antibodies isolated from B cells of COVID-19 survivors, fusion proteins, DARPin molecules (designed ankyrin repeat proteins), or single-domain antibodies (VHH). Many of these candidates target the RBD while few other molecules target different regions of the spike.
Some researchers have raised concerns regarding the current COVID-19 drug development efforts. Given the gaps in knowledge on the SARS-CoV-2 mechanism of action and the typically high viral mutation rates, targeting a single region may backfire and reduce the efficiency of the current treatment options. Placing all the selective pressure into a single variable region increases the risk of mutation and the emergence of drug-resistant strains.
Remarkably, this concern has been addressed in a recent study published in Science. In this study, scientists isolated B cells from dozens of recovered donors and found an extreme diversity in terms of epitope recognition. Moreover, the majority of the isolated antibodies did not recognize RBD, the preferred target of many candidate biotherapeutics.
Surprisingly, many of these antibodies were shown to bind the N terminal domain (NTD) of the S1 subunit. With an undefined function, the NTP region is hypothesized to recognize specific sugar moieties on the host’s cell surface and play an important role in the structural transition of the spike from the prefusion to the postfusion state. Moreover, the new study revealed that the anti-NTD antibodies showed a strong viral neutralizing activity despite not blocking the RBD.
This suggests that, contrary to previous studies, the NTD may serve as a critical epitope for neutralizing antibodies.
Concluding remarks
Almost 150 COVID-19 drugs are currently undergoing clinical trials, preclinical studies, or in the early development stages of drug discovery. The frontrunners in the race to develop effective treatments are anti-inflammatory drugs aimed at alleviated the most severe symptoms caused by the COVID-19 disease. A little behind are the specific anti-SARS-CoV-2 treatments, in many cases obtained from the plasma or peripheral blood mononuclear cells of COVID-19 recovered patients.
Both approaches have important limitations. On the one hand, the symptomatic treatments serve only to treat a restricted subgroup of patients. On the other hand, the anti-SARS-CoV-2 antibodies currently under development are narrowly focused on binding the RBD.
This narrow approach may reduce the drug’s usability in the long term, due to the exacerbate risk of emergence of drug-resistant SARS-CoV-2 strains. For this reason, it is unlikely that a single drug will solve the current pandemic. Instead, drug developers should consider co-developing antibody cocktails targeting distinct epitopes of the spike (RBD and NTD) and the nucleocapsid protein, the two most abundant structural proteins of SARS-CoV-2.
- Chi, X. et al. A neutralizing human antibody binds to the N-terminal domain of the Spike protein of SARS-CoV-2. Science. 2020: eabc6052. doi: 10.1126/science.abc6952
- Chinese Antibody Society. COVID-19 Antibody Therapeutics Tracker. Retrieved from https://chineseantibody.org/covid-19-track/
- Coperchini, F. et al. The Cytokine Storm in COVID-19: An Overview of the Involvement of the chemokine/chemokine-receptor System. Cytokine Growth Factor Rev. 2020; 53:25-32. doi: 10.1016/j.cytogfr.2020.05.003
- Horby, P. et al. Effect of Dexamethasone in Hospitalized Patients with COVID-19: Preliminary Report. medRxiv. June 22, 2020. doi: 10.1101/2020.06.22.20137273
- Silverman, E. Hospitals see shortages of a cheap steroid that one study says helps Covid-19 patients. Pharmalot. June 25, 2020. Retrieved from https://www.statnews.com/pharmalot/2020/06/25/covid19-coronavirus-dexamethasone-shortages/