Antibody production
Antibody production
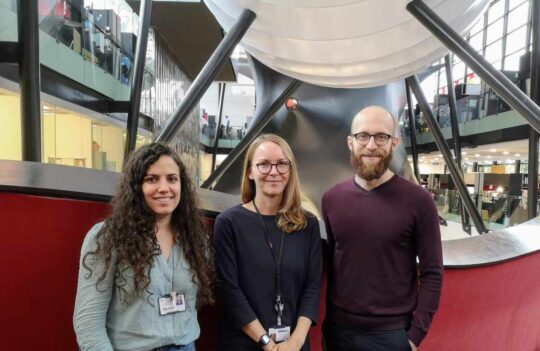
How the environment shapes immune system development during pregnancy – interview with Dr. Melanie Conrad
Dr. Melanie Conrad, head of the Reproductive Immunology Lab at the Charité Medical University in Berlin, Germany, has dedicated her career to understanding how genetics and the prenatal environment intertwine and influence allergy development. We recently talked with Dr. Conrad about her fascinating discoveries on pregnancy and the challenges she and her team have been tackling during the COVID-19 pandemic.
- ProteoGenix: Starting with your academic and professional journey, when did you become interested in reproductive immunology and allergy development?
- Was the work you did during your PhD related to the work you are doing now?
- Talking about your most recent work, we have seen a marked increase in the prevalence of allergic diseases like asthma. Some experts have called it the “allergy epidemic.” Throughout your career, what have you found to be the most plausible explanation for this devastating trend?
- How did you carry out these laboratory studies, and how did they differ from the prior epidemiological studies?
- Have you looked into the mechanistic aspects of this process?
- Your work serves as the proof of concept for the “hygiene hypothesis” that states that childhood exposure to microorganisms protects against allergic diseases. Could you associate this protective response with a specific protein from A. lwoffi?
- We could almost conclude that our urban houses are too clean.
- You revisited the topic of maternal influence on allergy development in one of your most recent publications. In this study, you assessed if there was a link between maternal asthma during pregnancy (a prevalent allergic condition) and asthma development in early life. What were the most important findings of this study?
- Do changes in glycosylation only happen when the mother is exposed to allergens?
- When the mother has a genetic predisposition for allergies, how can we protect the children from developing allergies as well?
- What can we do as individuals and collectively as a society to reduce the burden of this increase in allergies, especially during the prenatal stages and early life?
- Speaking of stress, you have recently launched a study to investigate the impact of stress in pregnancy during the COVID-19 pandemic. What motivated this study in the first place?
- How are you carrying out this study during these challenging times?
- Are there any other similar studies on this topic?
- What type of samples will you be collecting during this study?
- What results do you expect to find?
- Are you still recruiting women for your study?
- Are there any other interesting projects happening at your lab?
- And what are your goals for the next 10 years?
- Throughout your prolific career, what do you consider being your greatest achievements?

ProteoGenix: Starting with your academic and professional journey, when did you become interested in reproductive immunology and allergy development?
Dr. Melanie Conrad: I’m originally from Canada and pursued my PhD degree there in immunogenetics. During that time, my work involved a strong mix of genetics and immunology but, at some point, I gravitated more towards immunology and less towards genetics. When I finished my PhD, I intended to come to Germany to do a postdoc and then return to Canada. But then I got a position at Prof. Harald Renz’s lab in Marburg (Germany) where I studied pregnancy, immunology, and allergy development and found it fascinating.
The studies I conducted with Prof. Renz influenced my decision to go into the field of reproductive immunology. Since then, I have learned a lot and found just how intriguing pregnancy can be. There was a link between what happened to the mother during pregnancy and how that impacted the development of the child, and I wanted to learn more!
Was the work you did during your PhD related to the work you are doing now?
My PhD studies were not very much related to pregnancy. I was more focused on genetics, particularly on sequencing T cell receptor genes. Part of my PhD revolved around the comparative immunology study of gamma delta T cell receptors in cows. These cells showed a remarkable variability between different species and we wanted to know if it had any relationship with the placentation in different animals. The influence and role of these cells is still an ongoing and intriguing challenge in the field.
Talking about your most recent work, we have seen a marked increase in the prevalence of allergic diseases like asthma. Some experts have called it the “allergy epidemic.” Throughout your career, what have you found to be the most plausible explanation for this devastating trend?
In the past 50 years, scientists have noticed that the increase in allergic and autoimmune diseases has progressed at a quite rapid rate. At the same time, the prevalence of infectious diseases has been decreasing. That strong correlation led us to question if the decreased exposure to microbes in industrialized societies and urban environments could have a detrimental effect on our immune system development.
A series of epidemiological studies that looked into children growing up in traditional farming environments inspired our initial experiments. In these environments, children were in close contact with farm animals like cows. They drank raw cow milk containing lots of good bacteria, and they had daily contact with hay that generates lots of dust. This dust is typically full of environmental bacteria and frequently inhaled by the children.
These studies found a link between growing up in a traditional farming environment and having a decreased risk of getting asthma. Interestingly, they also found that if women carried out their pregnancy in this environment, their children also had a lower incidence of asthma. It was fascinating to even think that the environment the mother had been exposed to could influence the baby so much. And so, we set out to model this correlation in the lab.
How did you carry out these laboratory studies, and how did they differ from the prior epidemiological studies?
Epidemiological studies are excellent because they provide important insights into associations, but if you want to look at pregnancy at the cellular and chemical levels, you need to measure everything that’s happening in the fetus and the mother at regular intervals, and mouse models are exceptional for this.
At the beginning of the study, our colleagues went to several farming sites and vacuumed all surfaces of those houses so they could look into the microbial composition of the dust. They discovered that a single bacterial species predominated in these environments – Acinetobacter lwoffii. A. lwoffii are non-pathogenic bacteria, and we hypothesized that exposing pregnant mice to these bacteria would have a protective effect on their offspring. We tested this by treating pregnant mice intranasally with suspensions of A. lwoffii because this would mimic more accurately what would happen if mice inhaled dust from farming sites.
We had also a specific protocol for inducing asthma in the offspring that we could use to measure changes in the immune response and understand if these changes were somehow related to A. lwoffii exposure during pregnancy. What we found was that the offspring of mice that had been exposed to the bacteria had a much lower incidence of asthma compared to the offspring of the control group.
We were elated with these results because they were showing, for the first time, that we could duplicate these particular human epidemiological studies using a mouse model.
Have you looked into the mechanistic aspects of this process?
Yes! In another part of this study, we focused on the mechanistic aspects. To understand them, we used Toll-like receptor knockout mothers in our experiments. These receptors are vital to recognize bacteria and initiate the immune response. By removing them, we were ensuring the mothers could not mount an effective immune response to A. lwoffii.
In contrast to the original study, knockout mothers did not show an immune response against the non-pathogenic bacteria and, as a result, their offspring weren’t protected anymore against asthma. These results helped us show that there was a real and important correlation between the environment the mothers had been exposed to during pregnancy, the maternal immune response and asthma susceptibility in the offspring.
Your work serves as the proof of concept for the “hygiene hypothesis” that states that childhood exposure to microorganisms protects against allergic diseases. Could you associate this protective response with a specific protein from A. lwoffi?
Next we considered the possibility that this protective response was bacteria specific. For this reason, we tested the influence of other non-pathogenic bacterial components (Lactobacillus rhamnosus) on asthma protection in young mice. Interestingly, our studies with L. rhamnosus components also protected against asthma, indicating that the protection mechanism is not dependent on a single bacterial antigen but more likely the result of comparatively higher exposure to non-pathogenic bacteria in farming environments.
This explanation makes sense if we think of how excessively clean our houses are in the cities compared to the houses in farming environments. People on farms are exposed to a greater amount and a greater diversity of bacteria. That prolonged contact ends up challenging their immune systems frequently resulting in a type of immune “education”. The mechanisms by which this education occurs are still relatively unknown and is a subject of major interest in our laboratory.

We could almost conclude that our urban houses are too clean.
Perhaps we can! We are starting to realize that maybe it could be detrimental to disinfect every single surface of our homes so frequently as we typically do.
You revisited the topic of maternal influence on allergy development in one of your most recent publications. In this study, you assessed if there was a link between maternal asthma during pregnancy (a prevalent allergic condition) and asthma development in early life. What were the most important findings of this study?
We know that genetics plays a large role in asthma susceptibility. Typically, when both your parents have asthma, there is a high risk that you are going to inherit and manifest that trait. But in this study, we wanted to go further by unraveling the role of both genetics and environment in asthma development.
To understand this, we used a mouse model and induced asthma during pregnancy. We had a maternal control group and two additional groups that were exposed to different allergens: either casein (a milk protein) or ovalbumin (OVA – egg white protein). With these three groups, we wanted to test if the offspring of mothers that had experienced asthma exacerbation during pregnancy had a higher risk of developing asthma.
Surprisingly, we found that when the mother had an allergy to casein, but her offspring were allergic to OVA, there was only a little increase in asthma incidence that wasn’t significant compared to the control group. But when the mother and offspring were allergic to the same allergen, the offspring showed a significantly higher risk of developing asthma compared to the control group.
Examining this response more closely, we discovered that antibody glycosylation could explain these differences. Many scientists overlook the impact of glycosylation in inflammatory processes, but an antibody can be proinflammatory or anti-inflammatory depending on the glycans attached to their Fc regions.
When we measured the IgG antibodies generated by mothers allergic to OVA, we found their antibodies to be very proinflammatory with a low content of galactose and a low content of sialic acid. We then noticed their offspring had the same pattern of IgG glycosylation. Since these antibodies can be transferred across the placenta, the mothers who had suffered an allergic exacerbation could have transferred proinflammatory IgG across the placenta and this might dictate the immune system development in the offspring.
Do changes in glycosylation only happen when the mother is exposed to allergens?
Glycosylation is a very flexible process. If you have an infection or any type of inflammation, your antibody glycosylation patterns change, which makes them very susceptible to environmental influences. So understanding this mechanism becomes very important.
When the mother has a genetic predisposition for allergies, how can we protect the children from developing allergies as well?
If the mother has an allergy, this means she has genetic risk factors that are passed on to her children. In this case, one of the most important things we can do is avoid adding to those risk factors.
For instance, the use of antibiotics during pregnancy is considered a risk factor in allergy development because they change the mother’s gut microbiome (the types of bacteria that live in the intestine). Of course, I’m not in any way suggesting that pregnant women should not take any antibiotics during pregnancy. Antibiotics are, in many cases, essential and unavoidable.
However, now that we know of this risk, both the medical community and policymakers must reassess the way we prescribe antibiotics during pregnancy because doctors tend to overprescribe. We know for a fact that at least 25% of women take antibiotics during pregnancy mostly because of urinary tract infections. If we change the way we assess the severity of those infections to identify those women who really need these antibiotics, we might decrease the risk of asthma incidence in their children.
What can we do as individuals and collectively as a society to reduce the burden of this increase in allergies, especially during the prenatal stages and early life?
There’s still much we don’t know about the influence of environmental factors on the immune system and allergy development. So, I believe we need to redouble our efforts and learn as much as possible about these mechanisms to propose the best strategies for reducing asthma incidence in children.
We know that the microbiome of the mother plays a huge role in the baby’s immune system development. When the baby is born, the gut is first seeded with bacteria from the mother’s vaginal microbiome and afterward, during breastfeeding, with bacteria from the mother’s skin. What we can do right now to reduce allergy development is to ensure that pregnant women eat a healthy diet and exercise. Do the things that everybody already knows are necessary but have difficulties adhering to because of stress.
Of course, minimizing stress is very important, but not possible in some situations, especially now that we are in the middle of a pandemic.
Speaking of stress, you have recently launched a study to investigate the impact of stress in pregnancy during the COVID-19 pandemic. What motivated this study in the first place?
When lockdown first started all over the world, we all thought hard about what we could do to learn from this situation. During that time, I was lucky enough to connect with Prof. Catherine Lebel and her team from Canada who had just started a study to investigate the impact of the pandemic on maternal mental health and its outcome in children.
They called it the “Pregnancy during the pandemic” study and created a 45-minute survey to assess how COVID-19 was impacting pregnant women in Canada. It excited me to learn about their study and I contacted them to ask if my team and I could join. They were thrilled about this opportunity and in an amazing act of open collaboration, they sent their survey so we could implement it here in Europe.
We all thought this would be a great opportunity to assess the real impact of this pandemic on pregnant women. Different countries have different levels of COVID-19 infections, and governments are handling this crisis very differently. We believe this has a profound impact on the stress levels of the population. To conduct this study here in Europe, I reached out to some of my wonderful collaborators in the UK, and they helped me implement it in the UK in record time. It took us about a month and a half to get the proper ethical approval, and we opened our study in June 2020.
How are you carrying out this study during these challenging times?
We called our sister cohort EPPOCH-UK (Maternal mental health during the COVID-19 pandemic: Effect of the Pandemic on Pregnancy Outcomes and Childhood Health) and created a website where women could self-enroll www.eppoch-uk.org.
This study is open to all pregnant women in the UK. After enrolment, we ask these women to fill our 45-minute survey, and every month during pregnancy we send them a short follow-up survey to assess their stress levels and determine if they have been exposed to risk factors like antibiotics. When the baby is born, we collect their pregnancy information, namely details about the delivery, and then collect the postpartum information.
In the postpartum questionnaires, we focus not only on the maternal levels of stress but also on the baby’s health during the first few months of life and at 1 year of age. We are particularly interested in knowing if the baby has contracted any viral infection during that time because viruses represent an important risk factor for asthma development in children.
We plan to follow-up with the children until their first year of age and, in the meantime, continue applying for funding so we can extend the cohort up to 5 years of age. A 5-year window would be better to assess the real impact this pandemic will have on asthma and allergy development in children.
Are there any other similar studies on this topic?
Most of the studies during the pandemic revolve around the direct infection with SARS-CoV-2. For instance, we know some researchers are looking into the impact of COVID-19 infections in pregnant women. But there are very few studies that try to investigate the impact of social factors in pregnant women during the pandemic.
What type of samples will you be collecting during this study?
We will send sample collection kits to participants for a voluntary portion of our study, and these women will collect stool samples at the end of their pregnancy so we can study their gut microbiome. The same women will also be able to collect stool samples from their children so we can understand how the stress levels of the mothers correlate with microbiome diversity in their children.
Since our study relies on self-enrolment rather than enrolment through a clinic we cannot collect blood or breastmilk samples. However, aside from stool, we can also collect urine and hair samples. What is interesting about the hair samples is that we store cortisol, the stress hormone, in our hair. These samples are like tree core samples where we can associate certain sections of the hair with a certain month and then measure the levels of cortisol in each section. This will help us correlate the information we get from the surveys with the levels of biological stress hormones.
What results do you expect to find?
One difficulty in our study is that everyone is affected by the pandemic, so we don’t have a control group. To overcome this issue, we are going to stratify our participants into groups. This will be possible because we have validated surveys about their anxiety and depression that will be vital to separate them into low and high-stress categories.
I expect this study to reveal that women who self-reported high-stress levels during the pandemic will have a markedly distinct gut microbiome from the women who reported lower levels of stress. I also expect that the gut microbiome of the children will follow a similar pattern because they are so strongly influenced by maternal microbiomes.
Some prior studies have shown that maternal stress during pregnancy is a risk factor for childhood asthma development. We hope to provide additional insights on how maternal stress correlates with the microbiome and childhood asthma. Approximately 3000 women have already joined our study, and we are very excited about the results this cohort will generate.
Are you still recruiting women for your study?
During the first wave, we recruited from June until the end of August, and then we didn’t really close the recruitment, but we just stopped advertising it. Now that the second wave is starting all over the world, we have restarted our advertisement efforts and are we are already getting about 15 new enrolments per day, which is terrific!
Are there any other interesting projects happening at your lab?
Yes! We are about to start another interesting project that is also investigating the influence of the microbiome in the immune system.
As you know, laboratory mice are raised in incredibly sterile conditions which severely limit the diversity of their microbiomes. The price to pay for this limitation becomes clear when you compare studies made with laboratory mice and those assessing human populations. Mounting evidence shows laboratory mouse models sometimes do not accurately mimic humans. This is an important drawback because we use mice in so many fields and lines of research.
A researcher named Dr. Stephan Rosshart has recently tackled this challenge and published a paper with fascinating results in Science (2019). Rosshart took embryos of lab strains of mice with a specific genetic makeup and transplanted them into wild mice that he just collected from natural environments. Wild mice have a full complex microbiome and a very “competent” immune system because of being recurrently exposed to pathogens and environmental bacteria. Rosshart hoped the microbiome from the wild mice would be transferred to the embryos.
He called the resulting mice “wildings”, and he compared the results obtained in these mice with humans and lab mice. What he and his team found was surprising: the wildings could mimic human studies more accurately than laboratory mice ever could. This has important implications for many fields, including my field of research.
For this reason, we started a collaboration with him where we will take our models of pregnancy and protection against asthma and test them in wildling mice with fully functioning microbiomes.
And what are your goals for the next 10 years?
I want to keep my lab growing and keep researching pregnancy because there are still so many intriguing questions to answer. I also have a very clear vision for my lab because I know that, at some point, labs can get too big and that can end up being detrimental for supervision of students. I really want to be a great supervisor.
For the next 10 years, we will continue investigating what happens in the mother during pregnancy and what happens in the offspring during immune system development, before any allergy manifests.
But we will also start exploring other topics. Until now, we have based our work on what happens during pregnancy, what crosses the placenta, and how the fetus develops. But of course, immune system development is a complex process that starts during gestation and continues in the neonates.
In one of our current studies, we assess specifically what changes occur in the microbiome and immune system of newborn mice when the mothers are treated with antibiotics. Additionally, we will determine the impact of breastmilk on the immune system development of newborns. Studying this influence in mice has been considered very challenging for some time because of the difficulties in harvesting milk from lactating mice.
But we recently found a paper where researchers could achieve this by designing a breastmilk pump adapted to these small mammals. This inspired us to design our own breastmilk pump, and this simple innovation is now opening a new world of opportunities for future studies on the influence of lactation in microbiome and immune system development.

Throughout your prolific career, what do you consider being your greatest achievements?
The fact that I could start my own lab and that I have been able to keep my lab going and growing for the past years is, for the moment, my greatest achievement.
Most scientists can relate that academia is quite a tough field to remain in. This is especially true for women who, because of care roles, children, and other responsibilities, often experience obstacles that prevent them from thriving in this system.
This is clear just by looking at the number of women professors and comparing them to the number of men professors. The difference is staggering. The fact that I’m still here and still growing, despite all difficulties of academia, makes me very happy and proud.
You can follow Dr. Melanie Conrad’s latest research on her website at www.conradlab.net or on Twitter at @MLConradLab
- Conrad, M. L. et al. Maternal TLR signaling is required for prenatal asthma protection by the nonpathogenic microbe Acinetobacter lwoffii F78. J Exp Med. 2009; 206(13):2869-77. doi: 10.1084/jem.20090845
- Conrad, M. L. et al. Immunological approaches for tolerance induction in allergy. Curr Top Microbiol Immunol. 2011; 352:1-26. doi: 10.1007/82_2011_128
- Sodemann, E. B., Conrad, M. L. et al. Maternal asthma is associated with persistent changes in allergic offspring antibody glycosylation. Clin Exp Allergy. 2020; 50(4):520-531. doi: 10.1111/cea.13559